How Deep Tissue Massage Helps Manage Arthritis Pain

Living with arthritis often feels like a constant battle against joint stiffness and nagging pain. You’ve probably tried creams, pills, and maybe a few stretches, but what if a hands‑on therapy could ease the ache and improve mobility without a single pill? That’s where deep tissue massage steps in. Below is a plain‑spoken guide that explains what it is, how it works for arthritis, when it’s safe, and how to fit it into a broader pain‑management plan.
What is Deep Tissue Massage?
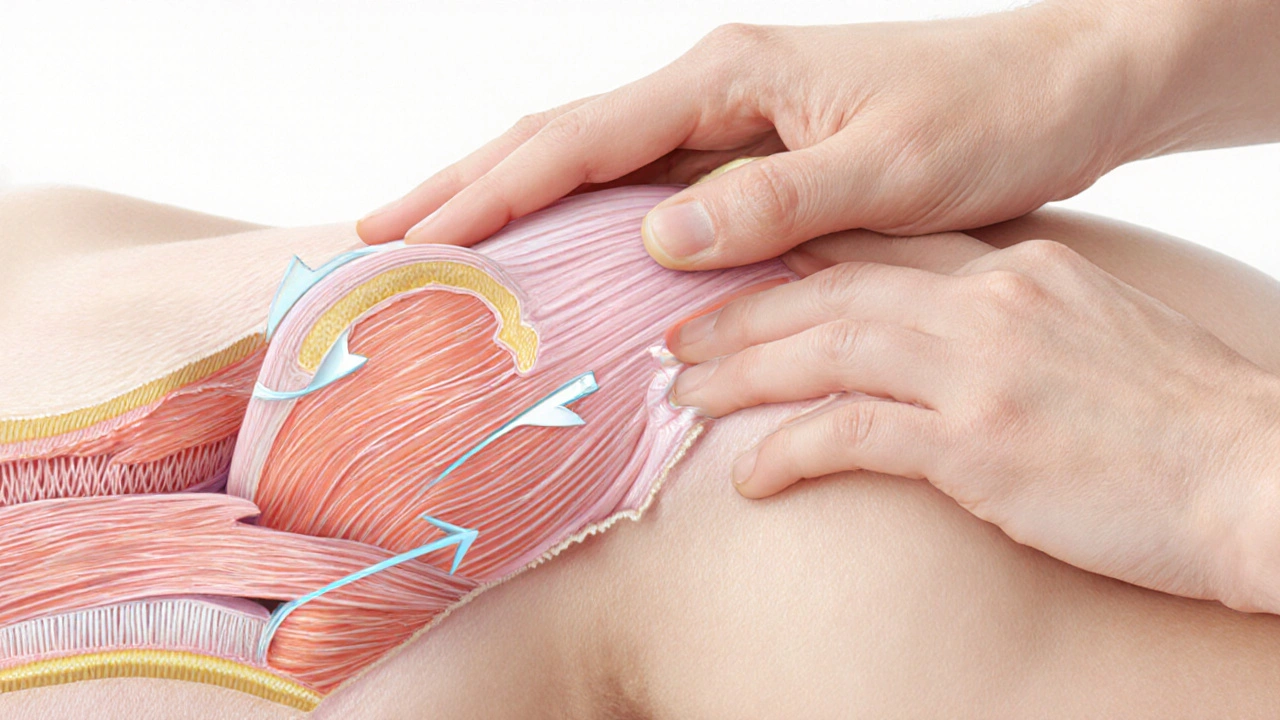
Deep Tissue Massage is a therapeutic technique that applies firm pressure to the deeper layers of muscle and connective tissue. It differs from a light Swedish rub‑down by targeting knots, adhesions, and chronic tension. The therapist uses slow strokes and focused pressure, often following the direction of muscle fibers, to break down scar tissue and improve blood flow.
Understanding Arthritis
Arthritis refers to the inflammation of one or more joints, causing pain, swelling, and reduced range of motion. Two main forms dominate the conversation:
- Osteoarthritis - wear‑and‑tear arthritis that erodes cartilage over time.
- Rheumatoid arthritis - an autoimmune condition that attacks the synovial lining, leading to joint erosion and systemic fatigue.
Both types share common symptoms: joint stiffness after inactivity, aching that worsens with use, and occasional swelling. While medication and exercise are front‑line treatments, many patients seek supplemental therapies to reduce reliance on drugs.
How Deep Tissue Massage Affects Arthritis Symptoms
When a therapist works on the deeper muscle layers, several physiological changes happen that can directly relieve arthritis discomfort:
- Improved blood circulation: Pressure forces fresh, oxygen‑rich blood into the treated area, helping clear metabolic waste that can irritate joints.
- Release of endorphins: The body responds to sustained pressure by releasing natural pain‑killers, which can dull the sharp ache associated with inflamed joints.
- Reduction of inflammation: Gentle, sustained pressure encourages the lymphatic system to drain excess fluid, lessening swelling in the joint capsule.
- Enhanced joint mobility: By loosening surrounding muscles, deep tissue work allows a broader range of motion, making daily tasks-like gripping a mug or climbing stairs-easier.
- Breakdown of adhesions: Over time, scar tissue can bind muscles to bone, pulling the joint out of alignment. Targeted pressure helps dissolve these adhesions, reducing abnormal stress on cartilage.
Research published in the Journal of Clinical Rheumatology (2023) found that participants receiving weekly deep tissue sessions reported a 30 % drop in pain scores after eight weeks, compared with a control group that only used NSAIDs.
When Deep Tissue Massage Is Appropriate for Arthritis
Not every arthritis patient should jump straight into a high‑intensity massage. Here’s a quick rule‑of‑thumb:
- Early‑stage Osteoarthritis: Generally safe if pain is mild to moderate. Focus on surrounding muscles rather than the joint itself.
- Moderate‑to‑severe Osteoarthritis: Use a lighter pressure approach; avoid direct pressure on bony spurs.
- Rheumatoid Arthritis during flare‑ups: Hold off until inflammation subsides. Gentle, low‑pressure techniques are better.
- Post‑surgical or post‑injection periods: Wait at least 48‑72 hours before the first deep session.
If you have active skin infections, uncontrolled diabetes, or blood‑clotting issues, check with a physician first. A skilled therapist will also ask about any recent imaging results to avoid aggravating fragile joints.
Integrating Massage with Other Arthritis Treatments
Deep tissue work shines when paired with a balanced plan:
- Physical therapy: Therapists prescribe specific stretches that keep muscles supple after a massage session.
- NSAIDs (e.g., ibuprofen): Use short‑term for flare‑ups; massage can reduce the needed dosage.
- Corticosteroid injections: Schedule massage at least a week after an injection to avoid bruising.
- Regular exercise: Low‑impact activities like swimming or cycling maintain joint health and amplify massage benefits.
The synergy works like a triangle: medication controls acute inflammation, exercise maintains joint function, and deep tissue massage improves tissue quality and pain perception.
Choosing the Right Therapist
Not all massage hands are created equal. Look for these credentials:
- Registered with the UK Register of Massage Therapists (UKRMT) or an equivalent body.
- Specific training in deep tissue techniques for musculoskeletal disorders.
- Experience working with arthritis patients-ask for references or case studies.
- Willingness to customize pressure levels based on your pain threshold.
A good therapist will also communicate clearly: they’ll explain each movement, check in about discomfort, and provide after‑care advice (like applying a warm compress).
DIY Self‑Massage Tips (When You Can’t Book a Session)
While nothing replaces a professional’s trained hands, a few safe self‑techniques can keep stiffness at bay:
- Use a tennis ball or foam roller on a wall. Gently roll the painful area for 1‑2 minutes, avoiding sharp pain.
- Apply a warm towel before self‑massage; heat relaxes muscles, making pressure more effective.
- Combine slow strokes with deep breathing-inhale through the nose, exhale through the mouth-to boost endorphin release.
- Limit each session to 10‑15 minutes; over‑working already inflamed tissue can worsen swelling.
Always stop if you notice sudden swelling, bruising, or a sharp stabbing sensation.
Which Massage Works Best for Arthritis? A Quick Comparison
| Massage Type | Pressure Level | Best for | Typical Session Length | Notes for Arthritis |
|---|---|---|---|---|
| Deep Tissue | Firm to strong | Chronic muscle tightness, moderate OA | 60‑90 min | Focus on surrounding muscles, avoid direct joint pressure. |
| Swedish | Light to moderate | General relaxation, early OA | 45‑60 min | Great for circulation, less effective on deep adhesions. |
| Aromatherapy | Light | Stress‑related flare‑ups | 45‑60 min | Essential oils can soothe, but pressure is mild. |
| Hot Stone | Moderate (heat‑based) | Muscle stiffness with mild joint pain | 60‑75 min | Heat improves flexibility; avoid if you have severe inflammation. |
Checklist: What to Discuss Before Your First Session
- Describe your arthritis type (OA or RA) and severity.
- Share any recent imaging reports or doctors’ notes.
- Ask the therapist how they will modify pressure for tender joints.
- Confirm the therapist’s sanitation practices-clean linens, hand washing.
- Set a clear post‑session plan: stretching, hydration, and a brief rest period.
Bottom Line
If you’re looking for a non‑pharmaceutical way to tame arthritis pain, deep tissue massage offers measurable relief for many sufferers. It works by boosting circulation, releasing endorphins, and loosening the muscles that pull on inflamed joints. Pair it with doctor‑approved medication, regular low‑impact exercise, and a qualified therapist, and you’ll likely notice a steadier improvement in daily comfort.

Is deep tissue massage safe for rheumatoid arthritis?
During active flare‑ups, the inflammation can make deep pressure painful and potentially worsen swelling. It’s safer to start with gentle, low‑pressure techniques and only move to deeper work once the flare has settled and a rheumatologist gives the green light.
How often should I get a deep tissue session?
Most clinicians recommend one session per week for the first six weeks, then reassess based on pain reduction and mobility gains. Some people transition to bi‑weekly maintenance after seeing stable improvement.
Can I combine deep tissue massage with heat therapy?
Yes-applying a warm compress before the massage helps relax muscles, making the deep strokes more effective. Just avoid overheating the joint itself; a 10‑minute warm towel is sufficient.
What red flags mean I should stop the massage?
Sharp stabbing pain, sudden swelling, bruising, or a feeling of joint instability are signs to pause and consult your doctor. Mild soreness is normal, but anything beyond that warrants a break.
Do insurance plans cover deep tissue massage for arthritis?
A few UK private health insurers reimburse manual‑therapy sessions when a physician’s prescription is attached. Check your policy details and ask the therapist for a receipt that includes the diagnosis code.




Conor Burke
October 22, 2025 AT 16:09Having dealt with osteoarthritis in my knees for several years, I can attest that pressure‑focused therapy can make a tangible difference. The deep‑tissue approach targets the fascia and muscle knots that often exacerbate joint stiffness. By improving local circulation, it assists in flushing metabolic waste, which otherwise contributes to discomfort. Moreover, the sustained pressure stimulates endogenous endorphin release, offering a natural analgesic effect. Personally, I schedule bi‑weekly sessions and complement them with a short stretching routine advised by my physiotherapist. It is crucial, however, to communicate any flare‑ups to the therapist so they can modulate the intensity. For individuals on anticoagulants, confirming safety with a physician beforehand is prudent. Overall, integrating deep tissue massage into a broader management plan has reduced my reliance on occasional NSAID use.
Melissa Garner
October 23, 2025 AT 08:13Wow, that sounds awesome! 🙌 I started a weekly deep‑tissue routine after my physio suggested it and I feel my hands aren’t as cramped anymore. The endorphin boost is real-my mood lifts right after each session. I also noticed that my morning stiffness shrank from two hours to barely thirty minutes. Don’t forget to tell your therapist right away if something feels too intense; they’ll dial it back. Trust me, a little bit of discomfort now pays off big later! 💪
Deb O'Hanley
October 24, 2025 AT 12:00I’m skeptical about fancy massages fixing arthritis, but I’ve tried a few and saw a slight improvement. The key is to avoid pressing directly on the joint when it’s inflamed. Stick to the muscles around it and keep the pressure moderate. If you feel sharp pain, stop immediately. Always check with your doctor first. Simple as that.
Patti Towhill
October 25, 2025 AT 15:46Totally get where you’re coming from, but I’ve actually felt a lot better after a gentle deep‑tissue session last month. My therapist focused on the calves and forearms, never the swollen knees, and the extra mobility was noticeable. It’s all about communication and listening to your body, you know?
Suman Jr
October 26, 2025 AT 18:33If you’re new to deep‑tissue massage and dealing with arthritis, start slow and let the therapist know your pain threshold. Many people find that a light warm‑up stretch before the session helps the muscles relax, making the deeper work more effective. Pair the massage with a short daily walk or swimming; the combined movement keeps the joints supple. Remember, consistency beats intensity-regular low‑impact sessions tend to yield steadier relief. You’ve got this, and every bit of reduced pain is a win.
David McAlister
October 27, 2025 AT 22:20Great points! 😊 Adding a brief 5‑minute foam‑roller routine at home can extend the benefits between appointments. Just roll slowly over the tender spots, stop if you hit a sharp sting, and breathe deeply. Also, staying hydrated helps flush out the metabolic waste that massage loosens up. Keep a simple log of your pain levels; you’ll be amazed at the trends you see over a few weeks.
Taylor Bayouth
October 29, 2025 AT 02:06Consistency is key.
Inaki Kelly
October 30, 2025 AT 05:53Exactly-making it a habit, even just 10 minutes a day, can add up fast 😊.
Jeremy Hunt
October 31, 2025 AT 09:40When considering deep tissue massage as part of an arthritis regimen, it helps to view it through a multi‑disciplinary lens rather than as a stand‑alone miracle cure. First, the therapist’s training level matters; certifications from recognized bodies ensure they understand the biomechanical stresses involved with compromised joints. Second, the timing of the session relative to medication intake can influence outcomes-receiving a massage shortly after an anti‑inflammatory dose may reduce post‑treatment soreness. Third, the pressure applied should be calibrated to the individual’s current flare status; during a mild flare a light to moderate approach is prudent, while in remission phases a firmer pressure can target chronic adhesions. Fourth, integrating targeted stretching immediately after the massage helps lock in the newly gained range of motion before the muscles tighten again. Fifth, maintaining a modest frequency-typically one session per week for six weeks-provides enough stimulus for physiological adaptation without overwhelming inflamed tissues. Sixth, complementing massage with low‑impact aerobic activity, such as water aerobics, enhances circulation and supports cartilage health. Seventh, nutrition plays a silent but vital role; omega‑3 fatty acids and antioxidant‑rich foods can synergize with the anti‑inflammatory effects of massage. Eighth, keeping an open line of communication with both your rheumatologist and massage therapist ensures that any changes in joint swelling or pain are promptly addressed. Ninth, documenting subjective pain scores and functional milestones creates an objective record that can guide future treatment adjustments. Tenth, be mindful of contraindications-active infections, recent surgeries, or severe osteoporosis require medical clearance before deep pressure is applied. Eleventh, for those with rheumatoid arthritis, starting with a gentle Swedish or lymphatic technique before progressing to deep tissue can prevent inadvertent exacerbation. Twelfth, many insurance plans, especially in the UK, will subsidize sessions if a physician’s prescription is attached, so inquire about coverage early on. Lastly, by viewing deep tissue massage as one component of a broader, evidence‑based strategy that includes medication, physical therapy, exercise, and lifestyle modifications, patients can maximize pain relief while preserving joint function for the long term. With patience and collaboration, many sufferers report a meaningful decline in daily pain and an uplift in quality of life.